FAQs
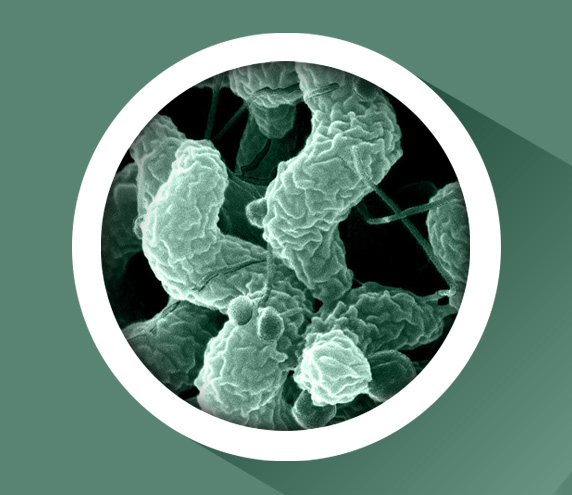
What is campylobacter?
Campylobacter is a group of bacteria that can cause infections in humans, often through food poisoning. Campylobacter is naturally occurring in the environment and can be found in livestock, domestic pets, and the countryside.
The two strains most commonly associated with infection in humans are campylobacter jejuni (C. Jejuni) and campylobacter coli (C. Coli).
How can it be avoided?
Good kitchen hygiene in handling of raw chicken and thorough cooking will eliminate the risk of campylobacter.
Kitchen hygiene includes the separation of meat and vegetables or ready to eat products, use of different utensils for preparing raw meat, and thorough washing of hands and utensils.
Campylobacter is killed by heat, so proper cooking completely eliminates this bacterium. Poultry and meat of all types, fish, eggs, and pastry products need to be heated through to 70C or higher and held at this temperature for at least two minutes.
What advice have consumers been given?
In supermarkets consumers will have seen new labelling on shelves and packs about kitchen hygiene. They will also have seen new roast-in-the-bag packaging that removes the need to handle chicken.
The Food Standards Agency has also run a campaign to raise awareness among consumers that there is no need to wash chicken, so as to avoid cross-contamination.
How many cases of campylobacter food poisoning are there?
In the UK the Food Standards Agency estimates there are approximately 280,000 cases of campylobacter food poisoning every year.
Around 70,000 GP visits are caused by campylobacter.
How does it get into chickens?
The exact way in which campylobacter gets into chickens is still widely debated.
Once campylobacter colonizes in the chicken, it can be carried through the production process.
What are the effects of campylobacter food poisoning?
In people, symptoms of campylobacter infection develop 2 to 5 days after ingesting the bacteria and infection may vary from mild diarrhoea to acute enteritis characterised by fever, headache, diarrhoea, and cramping abdominal pain.
The symptoms usually last for a few days, followed by recovery.
Campylobacter can have long-term effects for a minority of sufferers depending on the severity of infection; Irritable Bowel Syndrome (IBS), reactive arthritis or Guillain-Barré Syndrome. Deaths from campylobacter are very rare, and are generally associated with the vulnerable and those with underlying conditions.
What is the poultry industry doing?
The poultry industry and retailers are working hard to find interventions in the production chain that will reduce campylobacter.
This includes enhanced biosecurity on farms, new techniques for maintaining equipment, new technology in slaughterhouses, and novel ideas for packaging.
Who else is involved?
This is a united effort between farmers, producers, retailers, and government.
In 2009 the Joint Working Group was formed to tackle campylobacter, the members of which are the Food Standards Agency, British Poultry Council, British Retail Consortium, National Farmers Union, and Defra. This group has since overseen around 70 research projects looking at campylobacter; from its genetic make-up through to novel packaging.
It has not been until recent years that scientific techniques have been advanced enough for us start understanding the genetics of this bacterium. There are thousands of types of campylobacter and it is a genetically mobile organism, which means different types readily swap genetic material in order to adapt to changing conditions.
We have made significant leaps forward in knowledge and understanding since 2009, but are still a way off a complete solution. All the interventions we are progressing may contribute to an overall reduction, but the only intervention guaranteed to eliminate campylobacter remains thorough cooking.
For more information on what the industry and government are doing in the fight against campylobacter please visit www.campylobacter.org.uk